What is Pancreatic Surgery?
Pancreatic surgery is a critical procedure performed to address a variety of conditions affecting the pancreas, such as pancreatic cancer, chronic pancreatitis, or pancreatic cysts. The pancreas is an essential organ located behind the stomach, playing a central role in digestion and regulating blood sugar levels. Due to its vital functions, any disease or pancreatic conditions may have a profound impact on a patient’s overall health.
Pancreatic surgery often involves removing part or all of the pancreas to either treat cancer, alleviate chronic pain, or remove cysts. Since the pancreas is intricately connected with digestive and endocrine functions, pancreatic surgeries are complex and require careful consideration. When other treatments, such as medication or lifestyle changes, are not effective, surgery may offer the best chance for long-term relief or even survival.
Types of Pancreatic Surgery
Pancreaticoduodenectomy (Whipple Procedure)
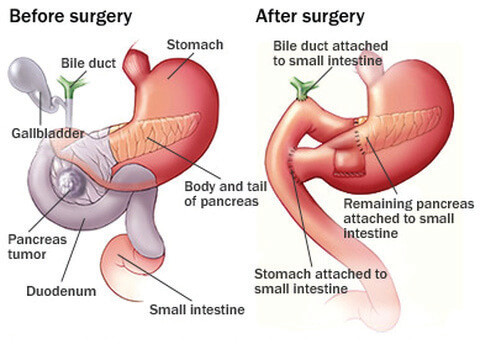
The Whipple procedure is the most common surgical intervention for pancreatic cancer, especially for those with tumours located in the head of the pancreas. It is a complex procedure that involves removing the head of the pancreas, the gallbladder, part of the bile duct, and sometimes a portion of the small intestine. After the removal, the digestive system is reconstructed to maintain its function.
Although the Whipple procedure is a major surgery, it offers hope for patients with pancreatic cancer or other conditions affecting the pancreas. For individuals diagnosed early, the surgery can significantly extend survival rates and provide an improved quality of life. Recovery, however, is typically longer due to the extensive nature of the surgery and the need for comprehensive post-operative care.
Distal Pancreatectomy with or without Splenectomy
A distal pancreatectomy, with or without splenectomy, is a surgical procedure to remove the body and tail of the pancreas, most commonly performed to treat pancreatic tumours, cysts, or other conditions affecting this part of the gland. In some cases, the spleen can be preserved, while in others it must be removed if the blood supply is shared or if disease involvement makes preservation unsafe. Dr Harald Puhalla performs distal pancreatectomy using a minimally invasive (laparoscopic or robotic) approach where appropriate, allowing for smaller incisions, reduced pain, and faster recovery compared with open surgery. The operation is carried out with meticulous attention to surrounding blood vessels and organs, and the decision to preserve or remove the spleen is made based on safety, anatomy, and the underlying condition, always with the goal of achieving the best clinical outcome for the patient.
Pancreatic Resection
Pancreatic resection is another type of surgery in which a part of the pancreas is removed. This surgery is generally recommended for patients with benign tumours, pancreatic cysts, or in some cases of pancreatic cancer. Unlike the Whipple procedure, pancreatic resection involves removing only the diseased portion of the pancreas while preserving the rest of the organ.
Pancreatic resections can be performed using minimally invasive techniques such as laparoscopic surgery, which uses small incisions and a camera to guide the surgeon. This method reduces the risk of infection, minimises scarring, and shortens recovery time compared to traditional open surgery. However, laparoscopic pancreatic resections are suitable only for certain types of conditions, and your surgeon will determine if this approach is right for you.
When is Pancreatic Surgery Needed?
Pancreatic surgery is often considered for pancreatic conditions when:
- Pancreatic Cancer or Tumours: If cancer or a tumour is diagnosed in the pancreas, surgery may be the best option to remove the tumour and prevent the disease from spreading. In cases of early-stage cancer, surgery like the Whipple procedure can offer a chance for long-term survival.
- Chronic Pancreatitis: Chronic pancreatitis is a painful and debilitating condition that leads to inflammation of the pancreas, often caused by long-term alcohol use, gallstones, or high triglycerides. If the condition doesn’t respond to medications or lifestyle changes, surgery may be required to remove the damaged part of the pancreas or to relieve pain.
- Pancreatic Cysts or Pseudocysts: Pancreatic cysts are fluid-filled sacs that can form within the pancreas. In some cases, they can become infected, bleed, or even turn cancerous. If a cyst causes complications or poses a risk of becoming cancerous, surgical removal may be necessary.
What to Expect Before and After Pancreatic Surgery
Before Surgery
Prior to any pancreatic surgery, a thorough evaluation is essential. This includes:
- Imaging tests such as CT scans, MRI, and ultrasound to locate tumours or cysts and assess the extent of disease.
- Blood work to assess overall health and liver function.
- A consultation with your surgeon to discuss the surgical procedure, risks, potential complications, and the recovery process. Your surgeon will ensure you understand what to expect and the lifestyle changes necessary for optimal recovery.
After Surgery
Post-surgery recovery depends on the type of procedure you undergo. For major surgeries like the Whipple procedure, recovery typically takes several weeks to months, and patients may require a hospital stay for monitoring and care.
In the initial stages of recovery, patients will need to:
- Follow a strict diet that gradually progresses from liquids to solid foods. Nutritional needs will be closely monitored to ensure proper digestion and absorption of nutrients.
- Avoid strenuous physical activities and follow physical therapy guidelines to regain strength.
- Hydration is critical, especially since pancreatic surgery can affect the body’s ability to process nutrients and fluids.
- Regular follow-up visits are essential to track progress and monitor for any potential complications, such as infections or digestive issues.
For less invasive surgeries, such as pancreatic resection, recovery may be quicker, with many patients returning to daily activities within 2-4 weeks.
Risks and Complications
As with any surgery, pancreatic surgery carries risks. These may include:
- Infection or bleeding
- Nutritional deficiencies (due to altered digestive function)
- Digestive issues such as difficulty absorbing nutrients
- Pancreatic leakage or fistula formation, which can occur after the removal of pancreatic tissue
While these risks are significant, the likelihood of complications can be reduced through careful pre-surgery evaluation, skilled surgical techniques, and a well-managed recovery plan.
Pancreatic surgery is a critical and life-saving treatment for various conditions affecting the pancreas, such as pancreatic cancer, chronic pancreatitis, and pancreatic cysts. The decision to undergo pancreatic surgery should be made in consultation with a qualified surgeon who can assess your specific condition and recommend the best course of treatment.
Whether undergoing the Whipple procedure, pancreatic resection, or other forms of pancreatic surgery, the ultimate goal is to improve your health, alleviate pain, and prevent further complications. While recovery can take time, with appropriate post-operative care and lifestyle changes, many patients go on to lead healthy and fulfilling lives.
Medical Information Disclaimer
The information provided in this blog about pancreatic conditions is intended for general educational purposes only and does not constitute medical advice. Please consult with your healthcare provider for a personalised treatment plan based on your specific condition.