Comprehensive Liver Tumor Treatment: Advanced Surgical and Chemotherapy Options for Optimal Outcomes and Personalized Care
If liver tumours require treatment, the management options can be surgery, chemotherapy or a combination of both. Despite the fact that surgery provides the best long term survival for most cancerous liver tumours, some are too advanced and can only be treated with systemic chemotherapy.
The treatment and management plan for patients with metastatic liver tumours is based on the site of the original primary cancer located elsewhere in the body.
Non-cancerous tumours are occasionally considered for surgery, if the patient is symptomatic.
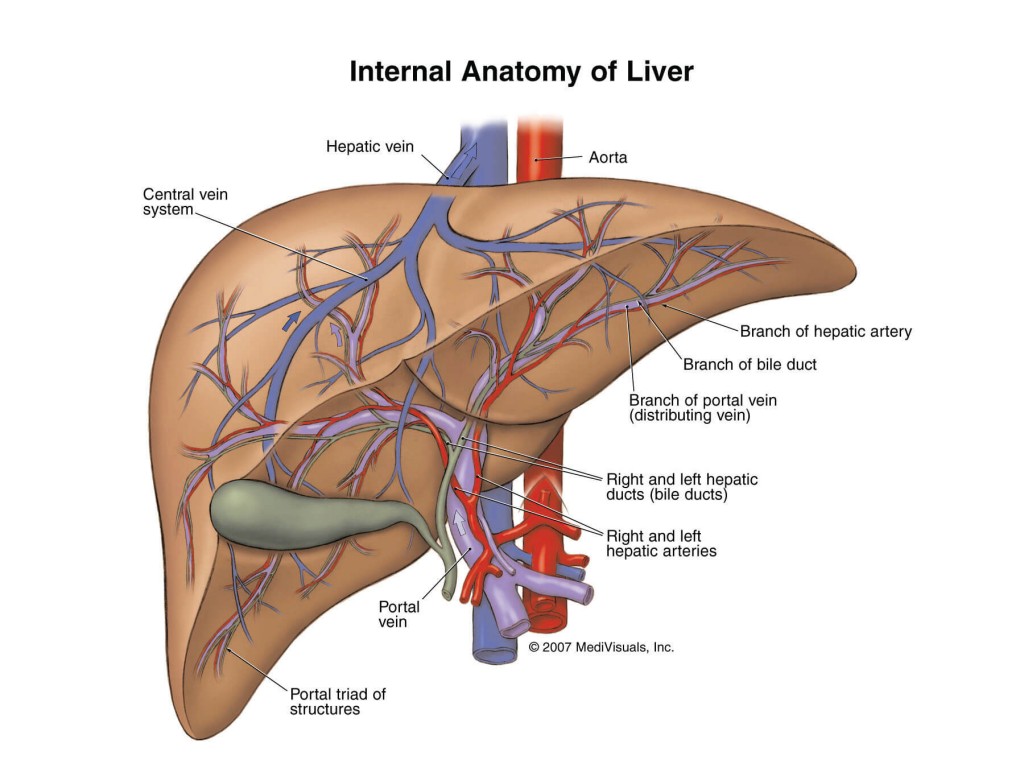
A liver resection is the surgical removal of the cancerous or diseased part of the liver. This type of surgery is the most effective treatment for patients with liver metastases from colorectal cancer limited to the liver.
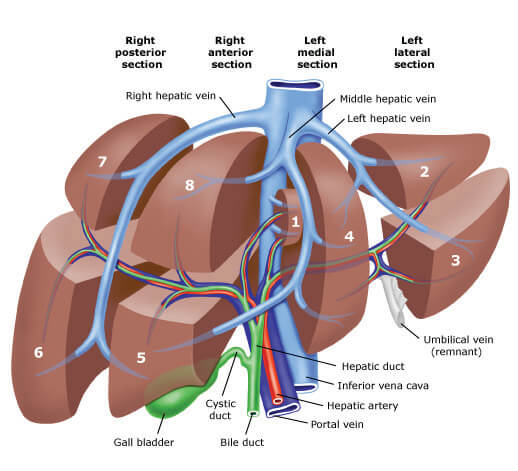
The liver is the only organ in the human body capable of re-growing after being partially removed. Because of this, up to 70-80% of the liver can be surgically removed, preserving enough functioning liver tissue to avoid liver failure, which can be fatal.
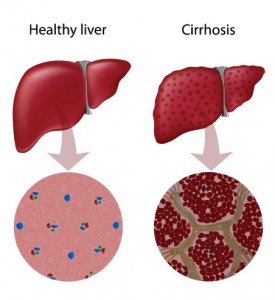
However, in patients with liver diseases (e.g. cirrhosis or fibrosis), more liver tissue needs to be left inside the patient as these diseases can reduce the functional capacity of the organ.
When possible, a liver resection can be performed by laparoscopic (keyhole) surgery which is a minimallyinvasive form of surgery that can potentially reduce patient recovery time compared with traditional surgery.
Liver surgery is a major operation that should be undertaken by an experienced surgeon. Mortality rates vary from 0.7-2.25% and can be higher in patients who have complications or existing liver disease.
The reported complications from liver surgery include:
It weighs approximately 1.5kg or about 2.2% of your total body weight.
The liver’s function can be reduced by chronic diseases such as hepatitis or by toxic substances (e.g. alcohol) which can cause fatty liver and scarring.
The liver has an essential role in:
A liver tumour is a solid mass within the liver which is formed when cells are aligned abnormally and start reproducing at an increased rate.
When a tumour has the capacity to invade locally or spread to other body parts, it is cancerous (malignant). Tumours that do not spread elsewhere in the body are benign.
The most common types of benign liver tumours include:
Cancerous liver tumours either originate in the liver (primary) or spread from other sites of the body to the liver (secondary).
Tumours that originate in the liver (primary) are often caused by by cirrhosis, which can be caused by viral hepatitis, excessive alcohol consumption, hemochromatosis, exposure to toxins and intake of anabolic agents. Another form of primary liver cancer originates from the bile ducts and is called cholangiocarcinoma. Rare forms of primary liver tumours are those arising from structures such as blood vessels, connective tissue (sarcoma) or blood/white cells (lymphoma/leukaemia).
Most cancerous tumours in the liver are secondary. Colorectal cancer is the most common cause of secondary liver cancer.
Metastases in the liver (the spread of a cancer from one organ to another) can also occur with breast, kidney, stomach, pancreas, connective tissue, melanoma and lung cancer.
Benign liver tumours are diagnosed by diagnostic imaging which can characterise the lesion and identify whether it is potentially cancerous. Blood tests and endoscopy are also used to confirm the non-cancerous character of this lesion.
Cancerous liver tumours are diagnosed using a series of tests to determine the stage (extent) of cancer of the liver as well as liver metastases.