Pancreas Surgery
Comprehensive Pancreatic Cancer Treatment: Surgical Options, Chemotherapy, and Personalised Care for Optimal Outcomes
Pancreatic Cancer Treatments
The treatment of pancreatic cancer varies and is dependent on whether the disease is confined to the pancreas or has extended into vital adjacent structures (e.g. vessels) or spread to other organs (e.g. liver).
Generally, surgery can be considered if the disease has not spread outside of the pancreas. In these cases, the cancer can be completely removed.
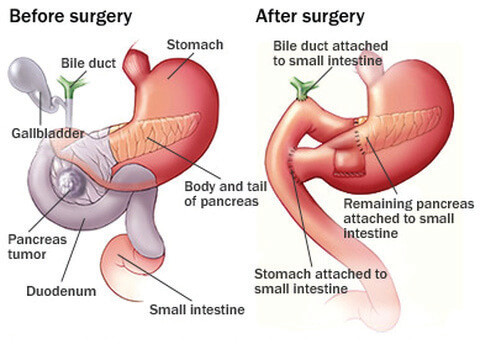
If the disease is in the pancreatic head, a “Whipple procedure” is performed, in which the pancreas is divided at the neck so the pancreatic head, the upper part of the small bowel and the lower part of the bile duct can be removed.
In order to reconstruct the digestive continuity, the small bowel is joined to the pancreas, then to the bile duct and also to the stomach.
If the lesion is more towards the tail of the pancreas, a distal pancreatectomy is indicated which sometimes can be performed laparoscopically. During this procedure, the pancreatic head stays behind and only the tail is removed. No reconstruction is necessary, but the spleen is often removed as well for oncological purposes.
In cases where surgery is not indicated, chemotherapy is used to control the cancer. If the cancer is locally advanced and is without distant metastases, chemotherapy may be able to shrink the lesion and then surgery may become an option.
Pancreas Resection Complications
Reported complications associated with pancreatic surgery include:
- Wound infection
- Clots
- Bleeding
- Leak from a joint (e.g. pancreas to the small bowel)
- Intra abdominal infection
- Bowel obstruction
Knowledge
The pancreas?
Located in the upper abdomen behind the stomach and the intestines, the pancreas is divided up into 3 sections: the head, body and tail.
In the centre of the pancreas runs a duct which delivers digestive enzymes into the small bowel. This pancreatic duct joins the bile duct to open into the small intestines. There are smaller groups of cells arranged like small islands scattered throughout the pancreas called the “Islets of Langerhans”.
The pancreas has two major functions:
- exocrine: production of enzymes for digestion of food
- endocrine: production of hormones, including some that regulate blood sugar
Which diseases affect the pancreas?
Pancreatitis
Pancreatitis is a disease characterised by inflammation of the pancreas. It can be either acute or chronic. The most common causes are gallstones, alcohol, high blood lipids, medications, high blood calcium, and autoimmune reactions; however, it is not infrequent that a cause is not found.
Symptoms include severe abdominal pain, swelling, fever and vomiting.
Acute pancreatitis is generally treated with supportive care followed by treatment of the underlying cause to prevent the pancreatitis from recurring. Most patients need to be in hospital and sometimes intensive care is needed. Most patients recover completely, but acute pancreatitis can be life threatening – especially if an infection occurs in the pancreas.
Occasionally, surgery or other procedures are needed to treat infection or fluid collections in or around the pancreas.
In most patients with chronic pancreatitis, the treatment is symptom orientated. This includes pain management, oral pancreatic digestive enzyme supplements, and nutritional support. Treatment of diabetes mellitus often requires insulin rather than tablets. The avoidance of alcohol is crucial.
Pancreatic tumours
The pancreas can contain cysts, which are fluid-filled areas lined by cells. Most are benign, but some of them are cancerous or contain lesions that can become cancer. Most tumours of the pancreas come from the cells that line the pancreatic duct. Rarely, cancers arise from thecells that make digestive enzymes or other cells within the pancreas.
About 1% of the pancreas tumours come from the hormone producing cells. These tumours are called neuroendocrine and can either make hormones such as excess insulin that cause symptoms (very low blood sugar, therefore it is called “functional”) or not produce hormones that cause any symptoms (“non-functional”).
Benign pancreatic tumours
Serous cystadenomas are usually found during imaging for other reasons. These lesions are filled with water like fluid and are almost always benign. The preferred treatment for this tumour is observation without surgery, unless the tumours are growing or there are associated symptoms (e.g. obstruction, pain).
Cancerous pancreatic tumours
Invasive ductal adenocarcinoma are the most common cancers of the pancreas. Unfortunately, patients often have no symptoms until the cancer is very advanced. Only about 10-20% of patients with invasive ductal adenocarcinoma are curable with surgical resection at the time of diagnosis.
Pancreatic neuroendocrine tumours arise from the hormone producing cells in the pancreas. The main symptoms are due to a pancreas mass (i.e. stomach or bile duct obstruction, pancreatitis), local invasion and hormone over production or nonspecific symptoms such as abdominal pain and weight loss. These tumours can be difficult to identify and are often diagnosed after they have already spread to other organs such as the liver.
Potential cancerous pancreatic tumour
Mucinous cystic neoplasm are large cystic lesions usually located in the body and tail of the pancreas. Most of them occur in women around the age of 55. These type of cancer can be aggressive and if possible, a complete surgical resection is the best treatment.
Intraductal papillary mucinous neoplasm (IPMN) is a cystic lesion which grows from the pancreatic duct system. IPMN produces thick mucin, which can cause symptoms similar to pancreatitis. IPMN are slightly more often seen in males. Surgical resection can be necessary or sometimes a close follow up may be considered for management.
How is pancreatic cancer diagnosed?
The following tests are used to diagnose or confirm pancreatic cancer:
- Blood tests to identify potential tumour markers and for general assessment
- Imaging (X-ray) to characterise lesions in the body which helps to differentiate in between non-cancerous and cancerous lesions. Various imaging techniques are used to diagnose or confirm tumours. Click here to read more about the various imaging techniques used to diagnose or confirm tumours.
- Biopsy





